Canadian Health Awareness Society : Resources
| Dental Health - Contents |
| Dental Health - Detail |
Is There a Link between Oral Health and Diabetes?
Dr. Ho C. Ma, Periodontist
We seldom realize how problems relating to our body can affect our oral health. During times of sickness, we consult a physician for treatment. Having dental problems, we seek our dentist for relief. Similarly, physicians and dentists tend to their own areas of expertise and responsibilities. However, in the past decade there has been an increase in communication and interaction between physicians and dentists, as research and studies have demonstrated that systemic and oral healths are highly correlated.
Studies have shown that periodontal patients are more susceptible to having diabetes. Likewise, diabetic patients are more likely to develop periodontal disease. If a patient is not treated timely, one’s condition could worsen: Periodontal disease can lead to tooth loss, whereas diabetes can cause complications in the heart, kidney, and cornea. Furthermore, research has demonstrated a possible link between periodontal disease and other systemic diseases, such as coronary heart disease, high blood pressure, thickening of the blood vessels, body weight gain, and low birth-weight babies. More studies are currently being conducted to confirm these points and to improve treatment modalities.
Healthcare professionals and an increasing amount of people have become more aware of the importance of oral health. This is especially true in how the link between oral and systemic diseases can act as a forewarning to severe consequences.
In light of this, it is important to understand what periodontal disease is, and how it develops.
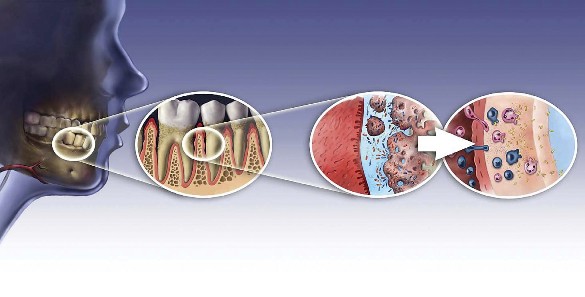
Fig.1: Progressive enlargement of the space between a tooth and gum tissues, illustrating the body’s reaction to invading bacteria with migration of the white blood cells and lymphatic cells to fight against the bacteria.
To state simply, periodontal disease is the inflammation of the gums resulting in the loss of bone support around the teeth in the oral cavity. The main cause is due to bacterial invasion, resulting in the breakdown of teeth supporting tissues. If we do not brush and floss our teeth regularly, we will begin to have a build-up of bio-film, referred to as dental plaque, accumulating on the teeth and gums. Plaque, which is invisible to the naked eye, is a thin, sticky, film material consisting of bacteria, along with their by-products, food debris, and muco-protein contained in the saliva. The bacteria survive easily by utilizing sugar from the food we eat as a nutrient source. Bacteria multiply quickly, growing to higher numbers in a short period of time. At the same time the bacteria produce an acidic and toxic by-product called endotoxin. This toxin, together with bacteria, can penetrate through gum tissues in the mouth into the surrounding blood vessels and migrate to different parts of our body via blood circulation.
Once bacterial invasion occurs in the gum tissues, the body reacts with an immunological response to protect itself. This is like a country sounding its alarm to defend itself from enemy. The circulating blood in the gum tissues release white blood cells, including a certain type called neutrophiles. These cells act like a front-line defence to neutralize the bacterial infection, by producing anti-inflammatory cell mediators such as interleukin-1 and tumor necrotic factor alpha. Subsequently, another kind of white blood cells called macrophages, move in to engulf and remove the bacteria. The body’s lymphatic system also plays an active role in the body’s immunological response to fight off the bacterial infection. (Fig.1)

Fig. 2: Severe inflammatory periodontal disease.
All of these immunological activities are being carried out in our body without our knowledge. We may, however, notice that our gum tissues become red, tender, swollen, and bleed easily, which are typical signs of periodontal disease.
If the bacterial build-up at this time is not rectified, periodontal disease will progress and worsen. The most obvious signs are deepening of the periodontal pockets, and further loss of supporting bone for the teeth. The degree and extent of bone loss vary; it can affect only a few teeth in a localized area, or it may involve all the teeth. If the bone loss is considered mild or moderate, the teeth may continue to function. However, if the bone loss becomes severe, the teeth will become mobile, difficult to be used for chewing, and may eventually fall off. (Fig. 2)
It is important to understand how periodontal disease and diabetes are related to each other. Research shows that during the active phase of inflammatory periodontal disease, a great number of white blood cells and lymphocytes are needed to combat the invading bacteria. This leads to a large build-up of inflammatory cells in the gum tissues, making our gums swell. The swelling may at times cause a traffic jam and impede regular blood flow in the gums. Without proper circulation, white blood cells will have difficulty in reaching the bacterial-infected areas, and the transport of blood sugar to the cells in the gum tissues will be reduced. As a result, the number of invading bacteria in tissues as well as the level of blood sugar in circulation remains high. This situation may lead to a worsening of the periodontal and diabetic condition for the patient. If this is not addressed properly, it can spiral into a vicious cycle.
As shown above, oral and systemic health is closely related. Assessing the condition of the oral cavity is just like peeping through a window to get a glimpse of the body’s physical condition.
Fig. 3: Attaining periodontal health subsequent to periodontal treatment
It is paramount to maintain adequate oral hygiene in order to make it harder for bacteria to build-up in the mouth. We should never take the basic habits of brushing and flossing lightly. In addition, regular dental check-ups and preventive treatment will further reduce the risk of periodontal disease. (Fig. 3). It may be too late to seek a dentist for treatment when a dental problem or periodontal infection is in the advanced stage. Similarly, if we find out we have diabetes, we should see a physician immediately for treatment.
Through the joint efforts of physicians, dentists and patients, periodontal disease and diabetes can be brought under control. With more research and studies currently underway, scientists will soon be able to find better ways to treat periodontal disease and diabetes for everyone’s benefit.
Studies have shown that periodontal patients are more susceptible to having diabetes. Likewise, diabetic patients are more likely to develop periodontal disease. If a patient is not treated timely, one’s condition could worsen: Periodontal disease can lead to tooth loss, whereas diabetes can cause complications in the heart, kidney, and cornea. Furthermore, research has demonstrated a possible link between periodontal disease and other systemic diseases, such as coronary heart disease, high blood pressure, thickening of the blood vessels, body weight gain, and low birth-weight babies. More studies are currently being conducted to confirm these points and to improve treatment modalities.
Healthcare professionals and an increasing amount of people have become more aware of the importance of oral health. This is especially true in how the link between oral and systemic diseases can act as a forewarning to severe consequences.
In light of this, it is important to understand what periodontal disease is, and how it develops.
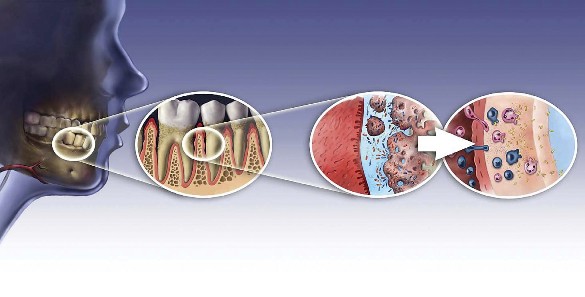
Fig.1: Progressive enlargement of the space between a tooth and gum tissues, illustrating the body’s reaction to invading bacteria with migration of the white blood cells and lymphatic cells to fight against the bacteria.
To state simply, periodontal disease is the inflammation of the gums resulting in the loss of bone support around the teeth in the oral cavity. The main cause is due to bacterial invasion, resulting in the breakdown of teeth supporting tissues. If we do not brush and floss our teeth regularly, we will begin to have a build-up of bio-film, referred to as dental plaque, accumulating on the teeth and gums. Plaque, which is invisible to the naked eye, is a thin, sticky, film material consisting of bacteria, along with their by-products, food debris, and muco-protein contained in the saliva. The bacteria survive easily by utilizing sugar from the food we eat as a nutrient source. Bacteria multiply quickly, growing to higher numbers in a short period of time. At the same time the bacteria produce an acidic and toxic by-product called endotoxin. This toxin, together with bacteria, can penetrate through gum tissues in the mouth into the surrounding blood vessels and migrate to different parts of our body via blood circulation.
Once bacterial invasion occurs in the gum tissues, the body reacts with an immunological response to protect itself. This is like a country sounding its alarm to defend itself from enemy. The circulating blood in the gum tissues release white blood cells, including a certain type called neutrophiles. These cells act like a front-line defence to neutralize the bacterial infection, by producing anti-inflammatory cell mediators such as interleukin-1 and tumor necrotic factor alpha. Subsequently, another kind of white blood cells called macrophages, move in to engulf and remove the bacteria. The body’s lymphatic system also plays an active role in the body’s immunological response to fight off the bacterial infection. (Fig.1)

Fig. 2: Severe inflammatory periodontal disease.
All of these immunological activities are being carried out in our body without our knowledge. We may, however, notice that our gum tissues become red, tender, swollen, and bleed easily, which are typical signs of periodontal disease.
If the bacterial build-up at this time is not rectified, periodontal disease will progress and worsen. The most obvious signs are deepening of the periodontal pockets, and further loss of supporting bone for the teeth. The degree and extent of bone loss vary; it can affect only a few teeth in a localized area, or it may involve all the teeth. If the bone loss is considered mild or moderate, the teeth may continue to function. However, if the bone loss becomes severe, the teeth will become mobile, difficult to be used for chewing, and may eventually fall off. (Fig. 2)
It is important to understand how periodontal disease and diabetes are related to each other. Research shows that during the active phase of inflammatory periodontal disease, a great number of white blood cells and lymphocytes are needed to combat the invading bacteria. This leads to a large build-up of inflammatory cells in the gum tissues, making our gums swell. The swelling may at times cause a traffic jam and impede regular blood flow in the gums. Without proper circulation, white blood cells will have difficulty in reaching the bacterial-infected areas, and the transport of blood sugar to the cells in the gum tissues will be reduced. As a result, the number of invading bacteria in tissues as well as the level of blood sugar in circulation remains high. This situation may lead to a worsening of the periodontal and diabetic condition for the patient. If this is not addressed properly, it can spiral into a vicious cycle.
As shown above, oral and systemic health is closely related. Assessing the condition of the oral cavity is just like peeping through a window to get a glimpse of the body’s physical condition.

Fig. 3: Attaining periodontal health subsequent to periodontal treatment
It is paramount to maintain adequate oral hygiene in order to make it harder for bacteria to build-up in the mouth. We should never take the basic habits of brushing and flossing lightly. In addition, regular dental check-ups and preventive treatment will further reduce the risk of periodontal disease. (Fig. 3). It may be too late to seek a dentist for treatment when a dental problem or periodontal infection is in the advanced stage. Similarly, if we find out we have diabetes, we should see a physician immediately for treatment.
Through the joint efforts of physicians, dentists and patients, periodontal disease and diabetes can be brought under control. With more research and studies currently underway, scientists will soon be able to find better ways to treat periodontal disease and diabetes for everyone’s benefit.
The Canadian Health Awareness Society is a registered non-profit organization. Our Mission is to promote health awareness on health issues for all Canadians by education, support and advocacy.