Canadian Health Awareness Society : Resources
| Others - Contents |
| Others - Detail |
Mechanical Back Pain
Dr. Lawrence Yang
With thanks to Dr Hamilton Hall
In the 2010 Global Burden of Disease Study, low back pain was one of the top 10 causes of highest DALY units worldwide.
It is estimated that 7 out of 10 people on earth will report back pain to their doctors at least once in their lives. It is estimated that every year, adults have a 1 in 20 chance of experiencing significant back pain. Back pain is often a frightening symptom for patients that causes very much suffering, anxiety, disability, and depression.
In the following paragraphs are some ideas about back pain developed by a leading orthopedic surgeon in Canada named Dr. Hamilton Hall. He works closely with leading physiotherapists and has pioneered back pain treatment methods and disseminated his teachings in many integrated back pain treatment centres around the world such as the Canadian Back Institute.
Treatment for the majority of back pains involve return to exercise and usual activities as soon as possible. It is generally never a good idea to spend prolonged periods in bed rest. “Movement is good medicine” as is true in most diseases. The one sign that you must see a doctor as soon as possible is sudden loss of ability to prevent bowel or bladder evacuation.
Back pains related to infections, inflammatory immune diseases, and cancer are constant pains which never go away no matter what position your body is in. True constant back pains are rare. They should be evaluated by a doctor as soon as possible.
“Mechanical back pain” is not life threatening, and not an emergency, but may cause significant suffering. Mechanical back pain is pain that changes in intensity with body movements and position. The majority of mechanical back pains are intermittent pains where the patient can find a position where the pain is reduced or goes away completely.
Mechanical back pain presents as what we call “leg dominant” symptoms or “back dominant” symptoms. Whether the pain is more severe below the buttock level or above the buttock level is what determines the dominant pain (ie. back or leg). Patients with pain worse in the legs (below the buttocks level) should be screened for nerve root irritation by their doctors.
A patient with leg dominant pains are the cases more likely to be treatable by surgery. However, not all cases will improve with surgery. Let your doctor decide which case should be evaluated by a surgeon. Back dominant mechanical pains are very rarely improved with surgery. Back dominant mechanical pains should not be treated with any surgery.
For this reason, the doctors usually would not order X-rays, CT-scans or MRIs for back dominant mechanical back pain patients. The large majority of back dominant and leg dominant pains can be made better with static or active positional exercises and the passage of time.
The following are some examples of static and active rest positions. At times, patience with repeated trials is required to discover which positions are most effective for each patient.
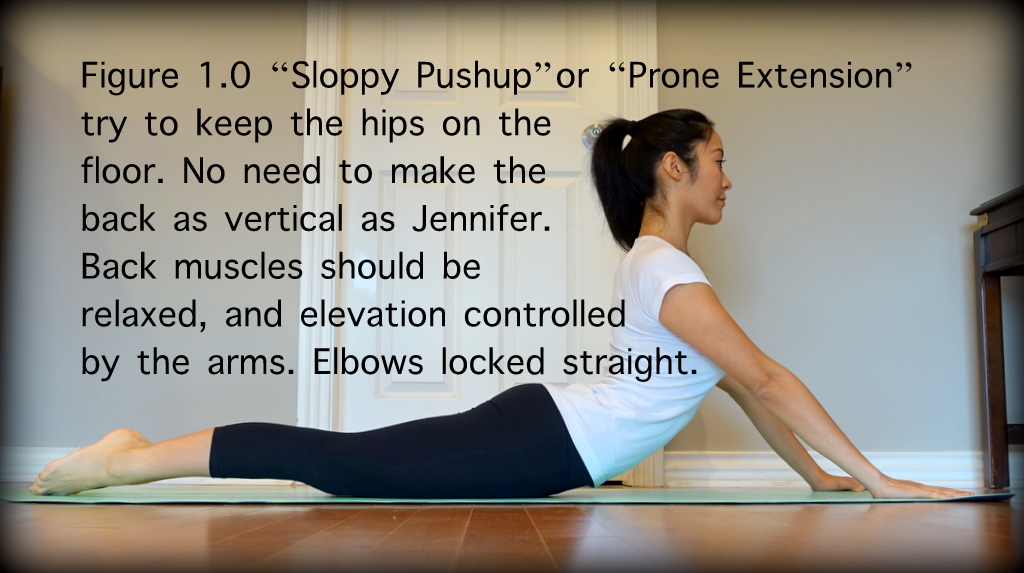
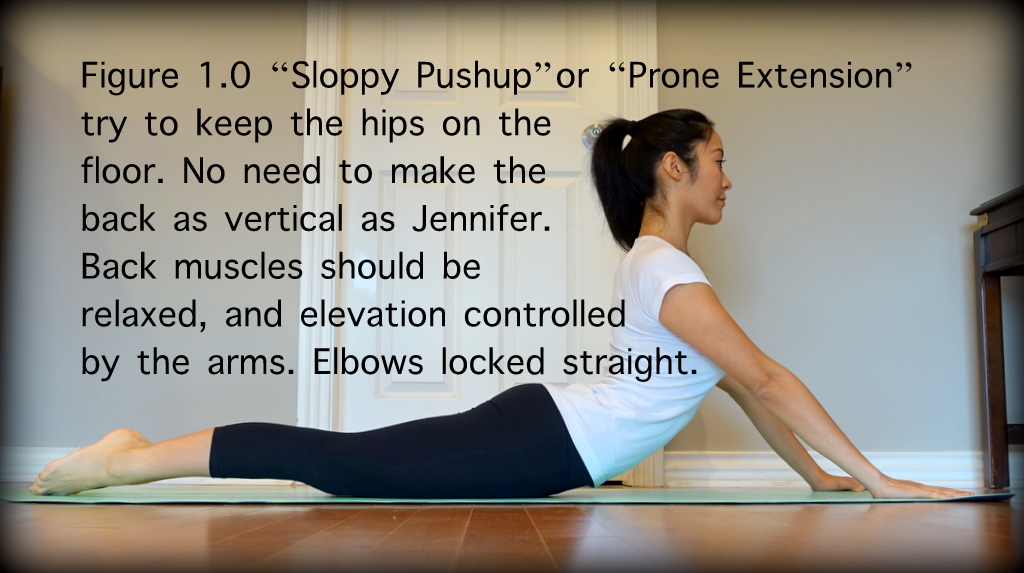
1.(figure 1.0) The “Sloppy Push-up” also known as “prone extension” or “prone lumbar extension”: Lie on clean floor or mat or carpet with abdomen side down and hands in front of your head about shoulder width apart. Keeping lower body and pelvis on the floor, extend the arms until the elbows are locked in extension and raise the upper body. The abdominal and back core muscles should not be activated and the upper body should be held up only by the structure of the shoulders and the locked elbows pushing through the palms of the hands on the floor or mat. With the elbows locked, rest in this position for a count of 5 to 10 seconds before lowering the upper body back down and repeat. As you can see, this movement requires some triceps strength. A modified version for those without adequate triceps strength can be to rest on the elbows instead of the palms of the hands.
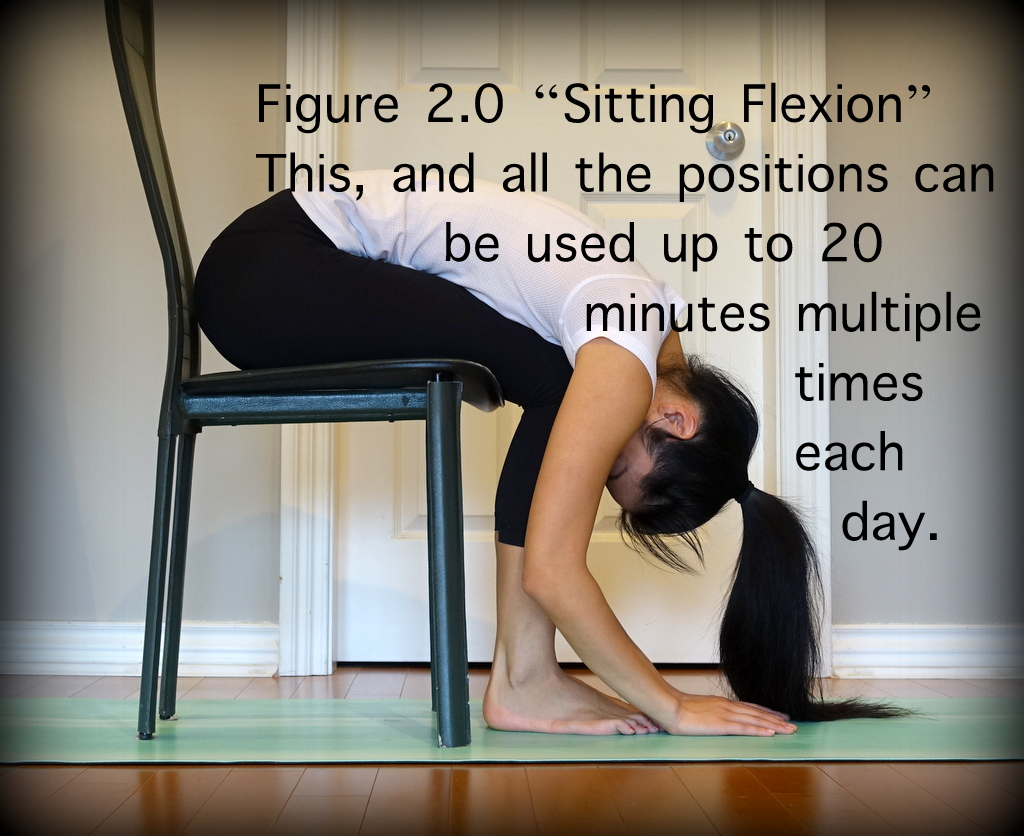
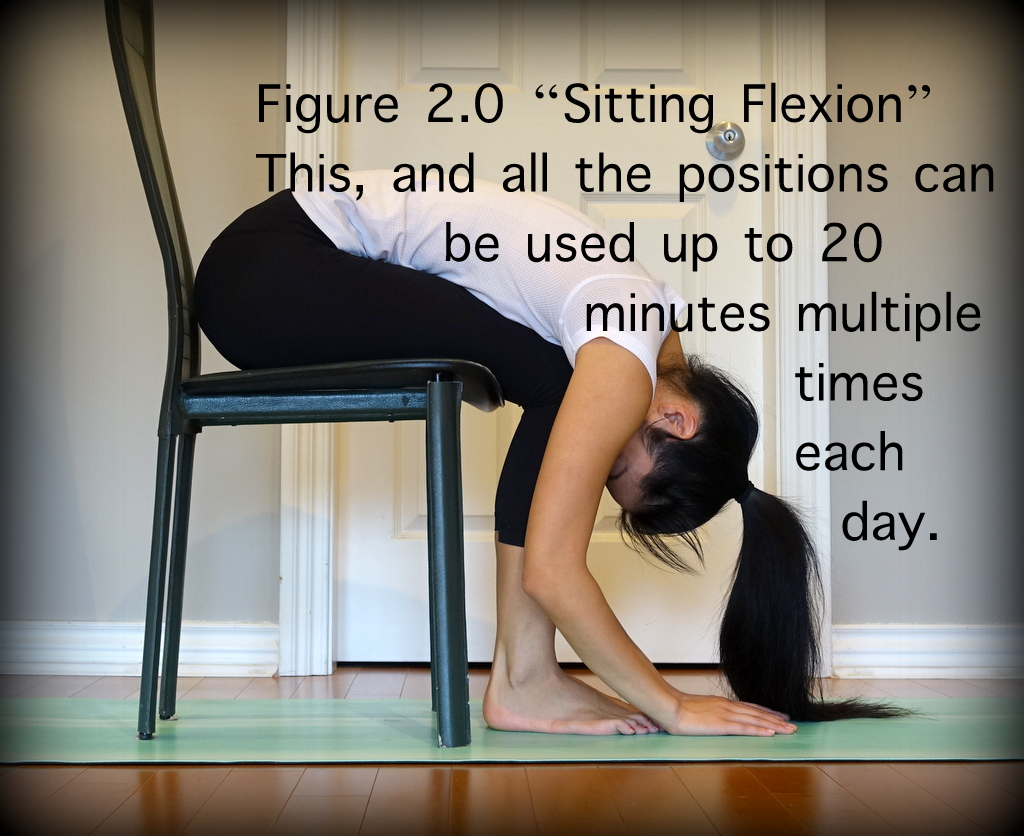
2.(figure 2.0) “Sitting flexion”: sitting on a firm chair or similar surface which allows one’s feet to comfortably rest flat on the floor, lean forward to rest your abdomen on your lap. Stay in this position if it reduces one’s typical back pain. when exiting this position, move slowly using one’s hands to push off one’s knees or thighs.
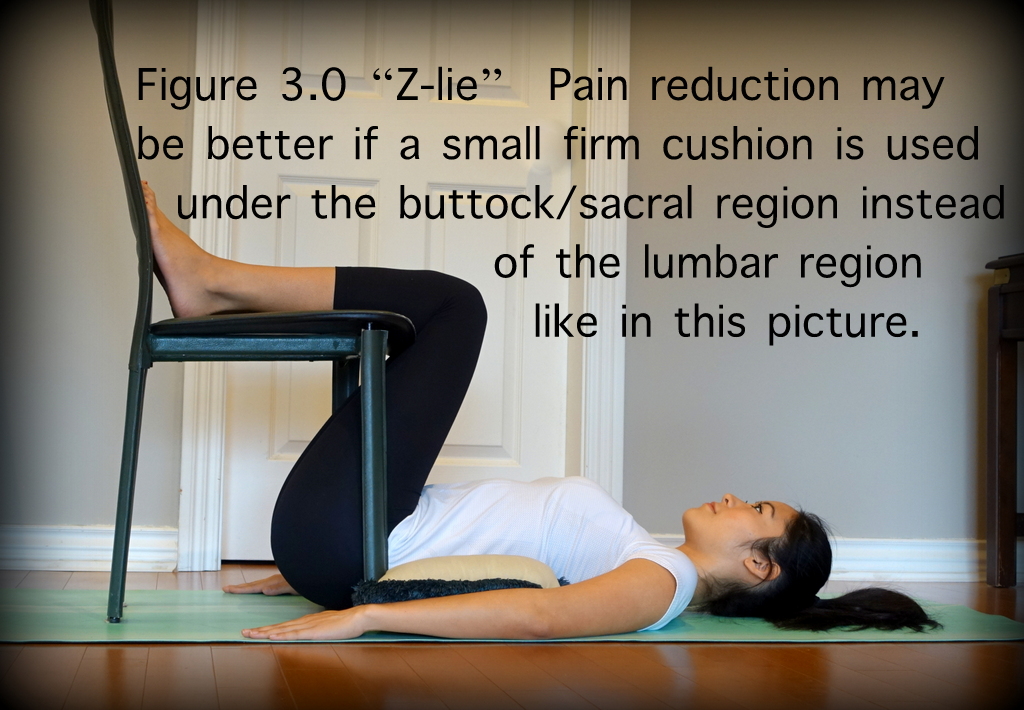
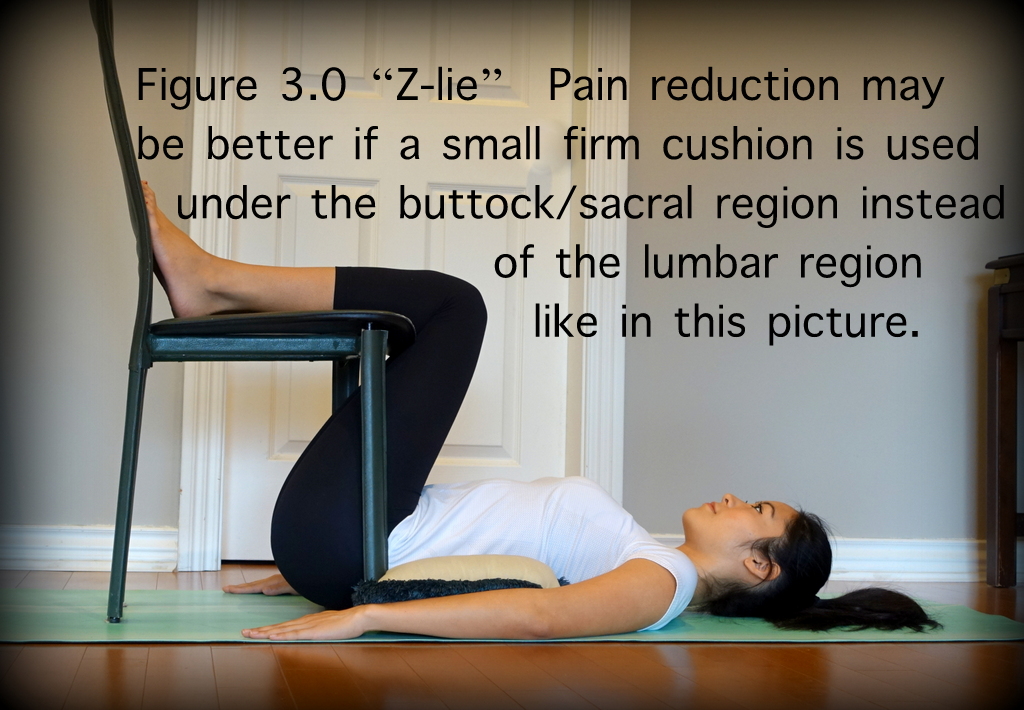
3.(figure 3.0) The “Z-lie”: lie with back flat on floor or mat and pillow under head and buttock. Flex hips and knees so the angles are more acute than 90 degrees and so the tibia, femurs, and spine form a “Z” shape. Rest the heels on a chair or other raised surface. Often the buttock will end up underneath the raised surface (chair seat) near the level of the ankles or the heels before good pain relief is realized.
4.(figure 4.0 and 4.1) The “Cat and Cow” positions in reference to yoga type positions.


The Saskatchewan Ministry of Health in Canada has made some excellent PDF files available on the world wide web depicting the remainder of the pain relieving positions researched and found to be beneficial by Dr. Hamilton Hall and his associates. You may find these PDF files by searching for: “Healthy Back Pattern”.
Positions that reduce mechanical back pain, allow a patient potentially to have control over when they feel pain. For example, if they are working as a cashier in the supermarket, during their breaks, they may find a location where they can practice the pain relieving positions. This is a method that takes practice, but in the long run, is beneficial for the patient’s psychology and also reduces risks of side effects that could be experienced from medications if pharmacotherapy was employed instead of resting positions.
These positions are to be used until pain levels allow the patient to advance to physiotherapy which targets strengthening of core muscles and other postural muscles. Once the severe pains of the back are reduced with the passage of time and the regular practice of pain relieving positions, the patients must immediately begin to strengthen their core and postural muscles.
In my experience, less than 1% of patients know how to strengthen their core muscles. I feel that any patient who suffers from back pain should immediately begin to educate themselves on how to strengthen core muscles.
There are thousands of exercises to strengthen core muscles, however, here are some simple low impact exercises to start with:
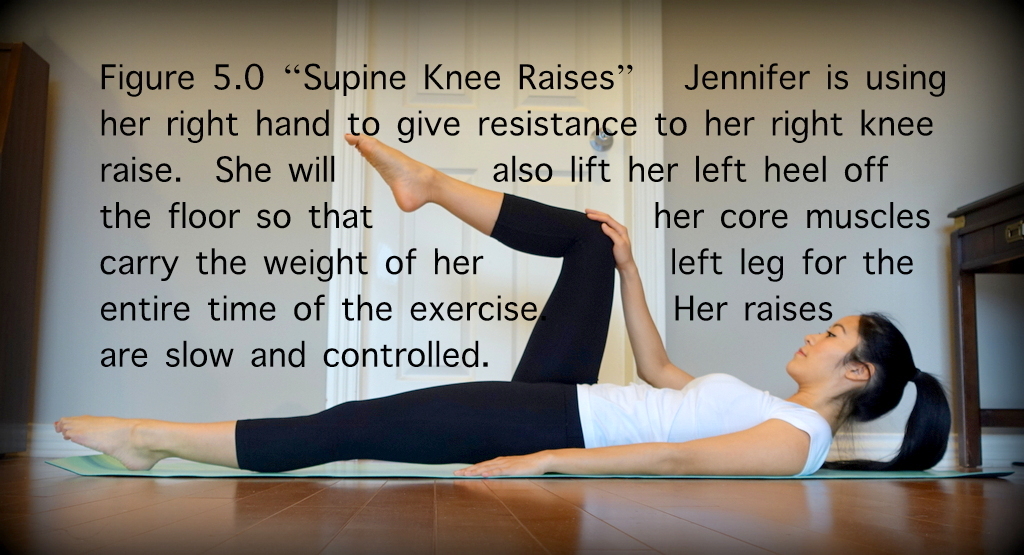
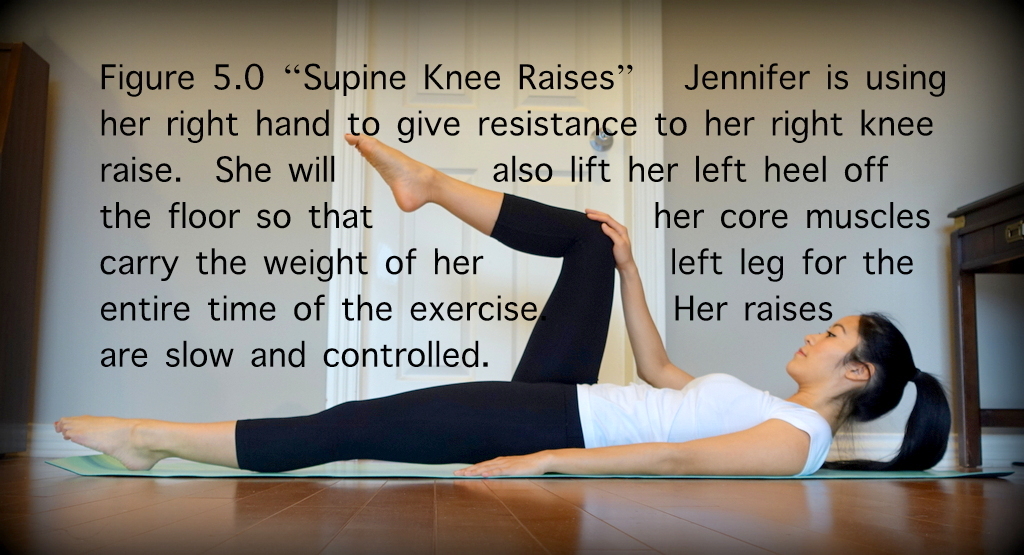
1.(figure 5.0) the “Supine knee raises”: Lie on back, arms along sides, palms down and just under lower back and butt. Press the upper of your back against the floor and extend legs outward, with heels about 3 inches above the floor. Keeping lower back against the floor, lift right knee toward chest. Your left leg should remain hovering above the floor. Hold, then straighten right leg to the starting position and repeat with left leg.
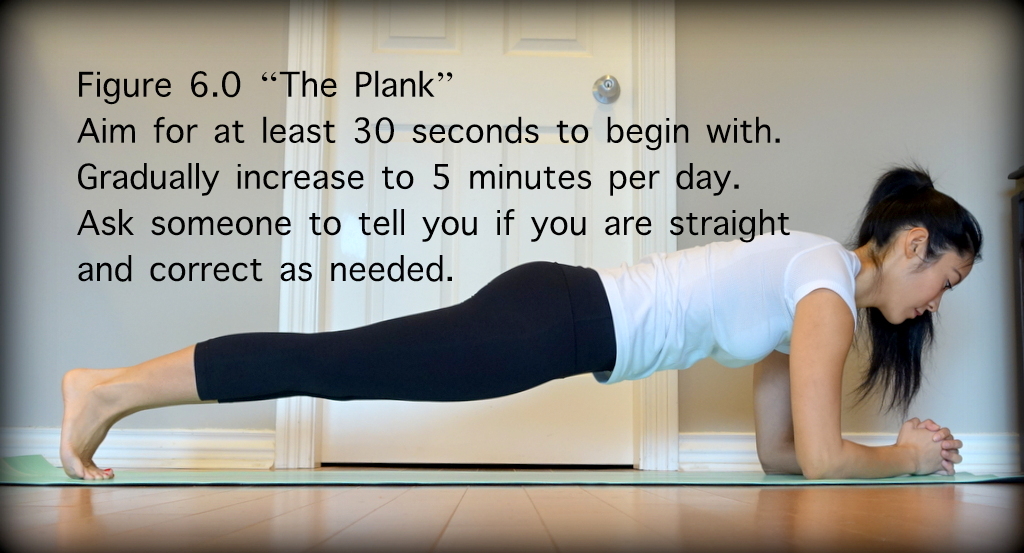
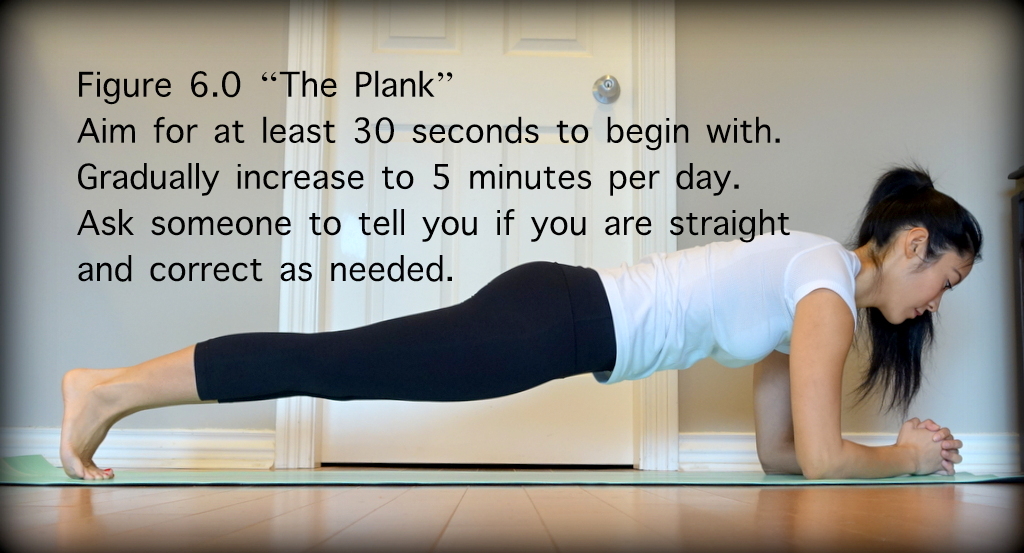
2.(figure 6.0) The “Plank”: Lie face-down on the floor with feet together and forearms on the ground. Draw abs in and tighten gluteals. Lift entire body off the ground until it forms a straight line from head to toe, resting on forearms and toes. Hold. Slowly return body to the ground, keeping chin tucked and back flat.
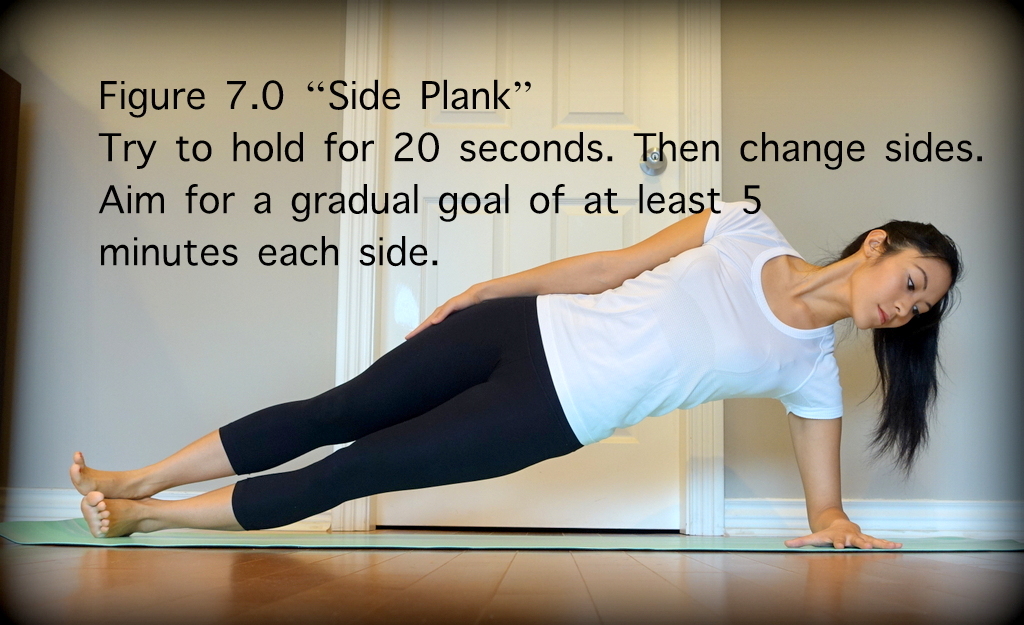
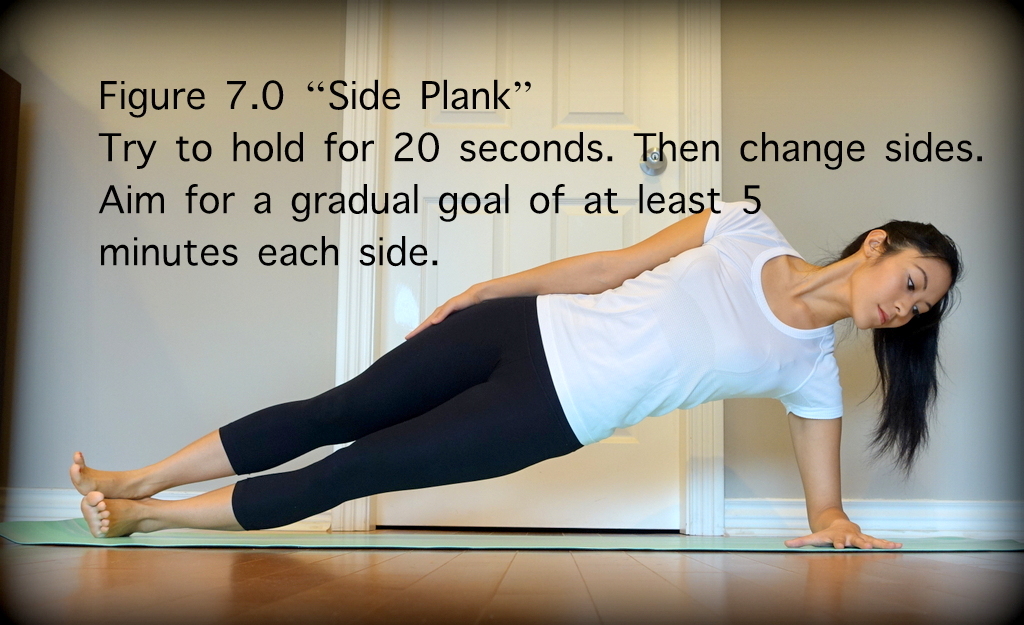
3.(figure 7.0) The “Side Plank”: Lie on side with lower arm bent at the elbow. Place lower elbow beneath shoulder and place upper hand on hip. Align ankles, hips, shoulders, and head. Push body toward the ceiling, balancing on the edge of your bottom shoe with one foot directly over the other.
4.(figure 8.0) The “Superman”: Lie face down on floor with arms in front of body, palms toward the ground. Draw navel in, tighten gluteus, and pinch shoulder blades together. Simultaneously lift arms, chest, and legs off the floor. Hold. Slowly return to ground, keeping chin tucked.

5.(figure 9.0) The “Body Weight Squat”: Stand with your feet slightly wider than your hips. Your toes should be pointed slightly outward – about 5 to 20 degrees outward. Look straight ahead and pick a spot on the wall in front of you. You'll want to look at this spot the entire time you squat, not looking down at the floor or up at the ceiling. While keeping a balanced posture with your spine as aligned as possible, lower your body by bending your knees until the angle of your knees is at least 90 degrees.
You may rise off your heels when standing and balancing in order to activate your gastrocnemius muscles. Your hands may rest on your hips or you may hold your hands in the air in front of you to assist your balance as you squat. Your buttock will naturally move backwards behind the level of your heels as you lower your trunk downwards. Then extend your knees lifting your trunk and upper body in a smooth controlled fashion maintaining balance throughout the movement. Repeat at least 20 times daily from standing to squatted position.

6.Swimming: Any type of swimming exercise can accentuate core muscle strength and flexibility. The buoyancy of the water assists greatly with relieving the effect of gravity on components of the joints in general which may be contributing to pains. Even if one cannot swim, walking and wading through water can improve health as the body adapts to the water resistance.
7.The “Stationary bicycle”: For many patients, bicycling offers a way to improve cardiovascular health which would otherwise not be realized due to weakness or pain from the back down through the legs. For these patients, a bicycle seat and handlebars allows an off-loading of the spine and legs onto the upper body (handlebars) and buttock (bicycle seat) which may be critical in assisting exercise which would be otherwise inhibited by pain or fatigue.
Much appreciation to Jennifer D. Lee for her valuable time and effort spent to produce and model the above figures for this publication.
These anti-inflammatory medications ought to be taken with at least a small amount of food. Systemic anti-inflammatory medications like ibuprofen and naproxen when taken by mouth should be avoided by patients with stomach ulcers or kidney filtration problems or who are pregnant. It is usually best to avoid taking the previously mentioned anti-inflammatories more than three days in a row to reduce side effects of prolonged exposure. Ask your doctor for more information regarding anti-inflammatories.
For patients with kidney or stomach problems where anti-inflammatories are not appropriate, acetaminophen is the pain reducer of choice. Acetaminophen is also available without a prescription. Acetaminophen is generally safe for all patients except those with advanced liver disease. It is best to avoid acetaminophen within 24hours of alcohol consumption. Ask your doctor for more information regarding acetaminophen.
Cannabinoid strains in the herbal form with 17% tetrahydrocannabinol and 1% cannabidiol have been shown anecdotally to be effective for severe pain at a dose of about 2 grams a day via vaporizer. There are also purified extracts with similar tetrahydrocannabinol and cannabidiol ratios in production which can be taken by mouth with oil based delivery systems. It is recommended to use the by mouth methods of consumption as they have no known pulmonary side effects. The time of onset of analgesia will be much delayed with the oral form versus the pulmonary form of intake.
The main negative side effects of marijuana are reduced reaction times which may increase risk of accidents, a risk of addiction, and of course the pungent odour of the herbal form which may result in social detriment. Patients under the age of 25 years are strongly advised to avoid cannabinoids due to evidence of risk of irreversible changes to the neurodevelopmental system.
In 99% of back pains, it is best to avoid opiate and opioid medications altogether. If a physician prescribes opiates or opioids, it is best to avoid using the analgesics for more than 3 days consecutively and for more than 14 days in a calendar month. The reason for this is generally unavoidable tolerance to the medications which will lead to eventual ineffectiveness of the medications and the resulting necessary uncomfortable withdrawals.
Withdrawals involve emotional dysregulation and worsened pain symptoms, amongst other uncomfortable symptoms. For some patients, opioid and opiate medications use can lead to addiction, social disorganization, severe social dysfunction, and even death by overdose or lethal combinations with chemicals such as alcohol.
Long term use of opioids has been proven to suppress life critical endogenous molecules like testosterone amongst other less known hormones. In some women, long term opiates and opioids can cause permanent infertility.
2. The New Back Doctor – Dec 1 1994 - Hall, Hamilton3. Links to the Saskatchewan Ministry of Health http://www.sasksurgery.ca/patient/spine.html
The Burden of Back Pain
The World Health Organization has a metric called the “disability-adjusted life year” (DALY) which is a measurement of disease burden on a human population. A DALY unit is expressed as the number of years lost due to ill-health, disability or early death.In the 2010 Global Burden of Disease Study, low back pain was one of the top 10 causes of highest DALY units worldwide.
It is estimated that 7 out of 10 people on earth will report back pain to their doctors at least once in their lives. It is estimated that every year, adults have a 1 in 20 chance of experiencing significant back pain. Back pain is often a frightening symptom for patients that causes very much suffering, anxiety, disability, and depression.
In the following paragraphs are some ideas about back pain developed by a leading orthopedic surgeon in Canada named Dr. Hamilton Hall. He works closely with leading physiotherapists and has pioneered back pain treatment methods and disseminated his teachings in many integrated back pain treatment centres around the world such as the Canadian Back Institute.
Treatment for the majority of back pains involve return to exercise and usual activities as soon as possible. It is generally never a good idea to spend prolonged periods in bed rest. “Movement is good medicine” as is true in most diseases. The one sign that you must see a doctor as soon as possible is sudden loss of ability to prevent bowel or bladder evacuation.
Mechanical Back Pain versus Other Back Pains
90 percent of back pain statistically is “mechanical back pain”. Statistically, 9% of back pain cases are related to inflammatory diseases and infections. Less than 1% of back pains are related to benign or malignant tumours. To diagnose which type of back pain you have, you must seek out a local health professional like a physiotherapist or medical doctor. Not every medical doctor is trained to evaluate back pains. Some of the specialist physicians best suited to evaluate back pains include neurosurgeons, orthopedic surgeons, physiatrists, sports medicine physicians, and family physicians.Back pains related to infections, inflammatory immune diseases, and cancer are constant pains which never go away no matter what position your body is in. True constant back pains are rare. They should be evaluated by a doctor as soon as possible.
“Mechanical back pain” is not life threatening, and not an emergency, but may cause significant suffering. Mechanical back pain is pain that changes in intensity with body movements and position. The majority of mechanical back pains are intermittent pains where the patient can find a position where the pain is reduced or goes away completely.
Mechanical back pain presents as what we call “leg dominant” symptoms or “back dominant” symptoms. Whether the pain is more severe below the buttock level or above the buttock level is what determines the dominant pain (ie. back or leg). Patients with pain worse in the legs (below the buttocks level) should be screened for nerve root irritation by their doctors.
A patient with leg dominant pains are the cases more likely to be treatable by surgery. However, not all cases will improve with surgery. Let your doctor decide which case should be evaluated by a surgeon. Back dominant mechanical pains are very rarely improved with surgery. Back dominant mechanical pains should not be treated with any surgery.
Do you require a radiological scan?
X-rays, CT-scans, and MRI studies are not recommended for any back dominant pains because it has been proven to worsen patient outcomes. The reason that patient outcomes are worse with X-rays, CT-scans, and MRI studies is that there will be some finding which does not in actuality correlate with the patient’s pain symptoms, however, the patient will become psychologically fixated on the “false positive” finding on the radiological study. Due to this psychological fixation on the “false positive” finding on the X-ray, CT-scan, or MRI, the patient will form an image of disability in their mind which will reduce their ability to participate in active rehabilitation. Most cases of severe chronic back pain require a high level of motivation to participate sufficiently in active rehabilitation in order to achieve a good recovery.For this reason, the doctors usually would not order X-rays, CT-scans or MRIs for back dominant mechanical back pain patients. The large majority of back dominant and leg dominant pains can be made better with static or active positional exercises and the passage of time.
Static Positional Exercises or Rest Positions for Reducing Pain:
“Static positional exercises” are positions where the patient rests and does not move (aside from usual automatic and breathing movements) that reduce a patient’s typical pain over 10 to 30 minutes. “Active positional exercises” are usually slow controlled movements that help to reduce a patient’s typical pain over time (usually months of regular exercises).The following are some examples of static and active rest positions. At times, patience with repeated trials is required to discover which positions are most effective for each patient.
1.(figure 1.0) The “Sloppy Push-up” also known as “prone extension” or “prone lumbar extension”: Lie on clean floor or mat or carpet with abdomen side down and hands in front of your head about shoulder width apart. Keeping lower body and pelvis on the floor, extend the arms until the elbows are locked in extension and raise the upper body. The abdominal and back core muscles should not be activated and the upper body should be held up only by the structure of the shoulders and the locked elbows pushing through the palms of the hands on the floor or mat. With the elbows locked, rest in this position for a count of 5 to 10 seconds before lowering the upper body back down and repeat. As you can see, this movement requires some triceps strength. A modified version for those without adequate triceps strength can be to rest on the elbows instead of the palms of the hands.
2.(figure 2.0) “Sitting flexion”: sitting on a firm chair or similar surface which allows one’s feet to comfortably rest flat on the floor, lean forward to rest your abdomen on your lap. Stay in this position if it reduces one’s typical back pain. when exiting this position, move slowly using one’s hands to push off one’s knees or thighs.
3.(figure 3.0) The “Z-lie”: lie with back flat on floor or mat and pillow under head and buttock. Flex hips and knees so the angles are more acute than 90 degrees and so the tibia, femurs, and spine form a “Z” shape. Rest the heels on a chair or other raised surface. Often the buttock will end up underneath the raised surface (chair seat) near the level of the ankles or the heels before good pain relief is realized.
4.(figure 4.0 and 4.1) The “Cat and Cow” positions in reference to yoga type positions.


The Saskatchewan Ministry of Health in Canada has made some excellent PDF files available on the world wide web depicting the remainder of the pain relieving positions researched and found to be beneficial by Dr. Hamilton Hall and his associates. You may find these PDF files by searching for: “Healthy Back Pattern”.
Positions that reduce mechanical back pain, allow a patient potentially to have control over when they feel pain. For example, if they are working as a cashier in the supermarket, during their breaks, they may find a location where they can practice the pain relieving positions. This is a method that takes practice, but in the long run, is beneficial for the patient’s psychology and also reduces risks of side effects that could be experienced from medications if pharmacotherapy was employed instead of resting positions.
These positions are to be used until pain levels allow the patient to advance to physiotherapy which targets strengthening of core muscles and other postural muscles. Once the severe pains of the back are reduced with the passage of time and the regular practice of pain relieving positions, the patients must immediately begin to strengthen their core and postural muscles.
Active Exercises for reducing risk of Back Pain:
It is my experience that most patients with chronic back pain have spent the majority of their lives neglecting their “core” and “postural” muscles. Of course, after developing chronic back pain, the entire body’s balance and musculature is weak and thus, developing said muscles becomes an even greater challenge. I wish all patients exercised their core from young childhood on a daily basis. Indeed we would have less disabled people if that were the case.In my experience, less than 1% of patients know how to strengthen their core muscles. I feel that any patient who suffers from back pain should immediately begin to educate themselves on how to strengthen core muscles.
There are thousands of exercises to strengthen core muscles, however, here are some simple low impact exercises to start with:
1.(figure 5.0) the “Supine knee raises”: Lie on back, arms along sides, palms down and just under lower back and butt. Press the upper of your back against the floor and extend legs outward, with heels about 3 inches above the floor. Keeping lower back against the floor, lift right knee toward chest. Your left leg should remain hovering above the floor. Hold, then straighten right leg to the starting position and repeat with left leg.
2.(figure 6.0) The “Plank”: Lie face-down on the floor with feet together and forearms on the ground. Draw abs in and tighten gluteals. Lift entire body off the ground until it forms a straight line from head to toe, resting on forearms and toes. Hold. Slowly return body to the ground, keeping chin tucked and back flat.
3.(figure 7.0) The “Side Plank”: Lie on side with lower arm bent at the elbow. Place lower elbow beneath shoulder and place upper hand on hip. Align ankles, hips, shoulders, and head. Push body toward the ceiling, balancing on the edge of your bottom shoe with one foot directly over the other.
4.(figure 8.0) The “Superman”: Lie face down on floor with arms in front of body, palms toward the ground. Draw navel in, tighten gluteus, and pinch shoulder blades together. Simultaneously lift arms, chest, and legs off the floor. Hold. Slowly return to ground, keeping chin tucked.

5.(figure 9.0) The “Body Weight Squat”: Stand with your feet slightly wider than your hips. Your toes should be pointed slightly outward – about 5 to 20 degrees outward. Look straight ahead and pick a spot on the wall in front of you. You'll want to look at this spot the entire time you squat, not looking down at the floor or up at the ceiling. While keeping a balanced posture with your spine as aligned as possible, lower your body by bending your knees until the angle of your knees is at least 90 degrees.
You may rise off your heels when standing and balancing in order to activate your gastrocnemius muscles. Your hands may rest on your hips or you may hold your hands in the air in front of you to assist your balance as you squat. Your buttock will naturally move backwards behind the level of your heels as you lower your trunk downwards. Then extend your knees lifting your trunk and upper body in a smooth controlled fashion maintaining balance throughout the movement. Repeat at least 20 times daily from standing to squatted position.

6.Swimming: Any type of swimming exercise can accentuate core muscle strength and flexibility. The buoyancy of the water assists greatly with relieving the effect of gravity on components of the joints in general which may be contributing to pains. Even if one cannot swim, walking and wading through water can improve health as the body adapts to the water resistance.
7.The “Stationary bicycle”: For many patients, bicycling offers a way to improve cardiovascular health which would otherwise not be realized due to weakness or pain from the back down through the legs. For these patients, a bicycle seat and handlebars allows an off-loading of the spine and legs onto the upper body (handlebars) and buttock (bicycle seat) which may be critical in assisting exercise which would be otherwise inhibited by pain or fatigue.
Much appreciation to Jennifer D. Lee for her valuable time and effort spent to produce and model the above figures for this publication.
Medications:
Medications are not a necessary part of back pain management, but they may assist in the patient’s ability to participate in muscle development. Anti-inflammatory medications like ibuprofen and naproxen are often the most affordable pain reducing medications for back pain. In most countries, ibuprofen and naproxen are available without a prescription. These anti-inflammatory medications ought to be taken with at least a small amount of food. Systemic anti-inflammatory medications like ibuprofen and naproxen when taken by mouth should be avoided by patients with stomach ulcers or kidney filtration problems or who are pregnant. It is usually best to avoid taking the previously mentioned anti-inflammatories more than three days in a row to reduce side effects of prolonged exposure. Ask your doctor for more information regarding anti-inflammatories.
For patients with kidney or stomach problems where anti-inflammatories are not appropriate, acetaminophen is the pain reducer of choice. Acetaminophen is also available without a prescription. Acetaminophen is generally safe for all patients except those with advanced liver disease. It is best to avoid acetaminophen within 24hours of alcohol consumption. Ask your doctor for more information regarding acetaminophen.
Cannabinoid strains in the herbal form with 17% tetrahydrocannabinol and 1% cannabidiol have been shown anecdotally to be effective for severe pain at a dose of about 2 grams a day via vaporizer. There are also purified extracts with similar tetrahydrocannabinol and cannabidiol ratios in production which can be taken by mouth with oil based delivery systems. It is recommended to use the by mouth methods of consumption as they have no known pulmonary side effects. The time of onset of analgesia will be much delayed with the oral form versus the pulmonary form of intake.
The main negative side effects of marijuana are reduced reaction times which may increase risk of accidents, a risk of addiction, and of course the pungent odour of the herbal form which may result in social detriment. Patients under the age of 25 years are strongly advised to avoid cannabinoids due to evidence of risk of irreversible changes to the neurodevelopmental system.
In 99% of back pains, it is best to avoid opiate and opioid medications altogether. If a physician prescribes opiates or opioids, it is best to avoid using the analgesics for more than 3 days consecutively and for more than 14 days in a calendar month. The reason for this is generally unavoidable tolerance to the medications which will lead to eventual ineffectiveness of the medications and the resulting necessary uncomfortable withdrawals.
Withdrawals involve emotional dysregulation and worsened pain symptoms, amongst other uncomfortable symptoms. For some patients, opioid and opiate medications use can lead to addiction, social disorganization, severe social dysfunction, and even death by overdose or lethal combinations with chemicals such as alcohol.
Long term use of opioids has been proven to suppress life critical endogenous molecules like testosterone amongst other less known hormones. In some women, long term opiates and opioids can cause permanent infertility.
Conclusion:
To summarize, most back pains require physical activity and creative rest positions and patience to maximize recovery speed. Seeking the help of a fitness trainer or physiotherapist or kinesiologist or physician is highly recommended for anyone with back pain.The Canadian Health Awareness Society is a registered non-profit organization. Our Mission is to promote health awareness on health issues for all Canadians by education, support and advocacy.
References:
1. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet, 2012, 380(9859):2163- 96. doi: 10.1016/S0140-6736(12)61729-2. Erratum in: Lancet, 2013, 381(9867):628. Al Mazroa, Mohammad A.2. The New Back Doctor – Dec 1 1994 - Hall, Hamilton3. Links to the Saskatchewan Ministry of Health http://www.sasksurgery.ca/patient/spine.html